
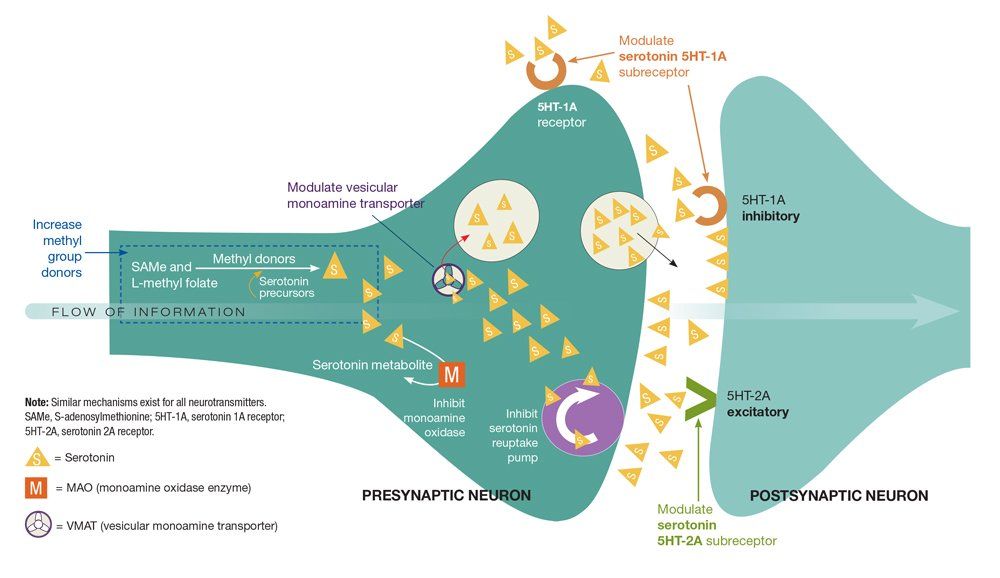
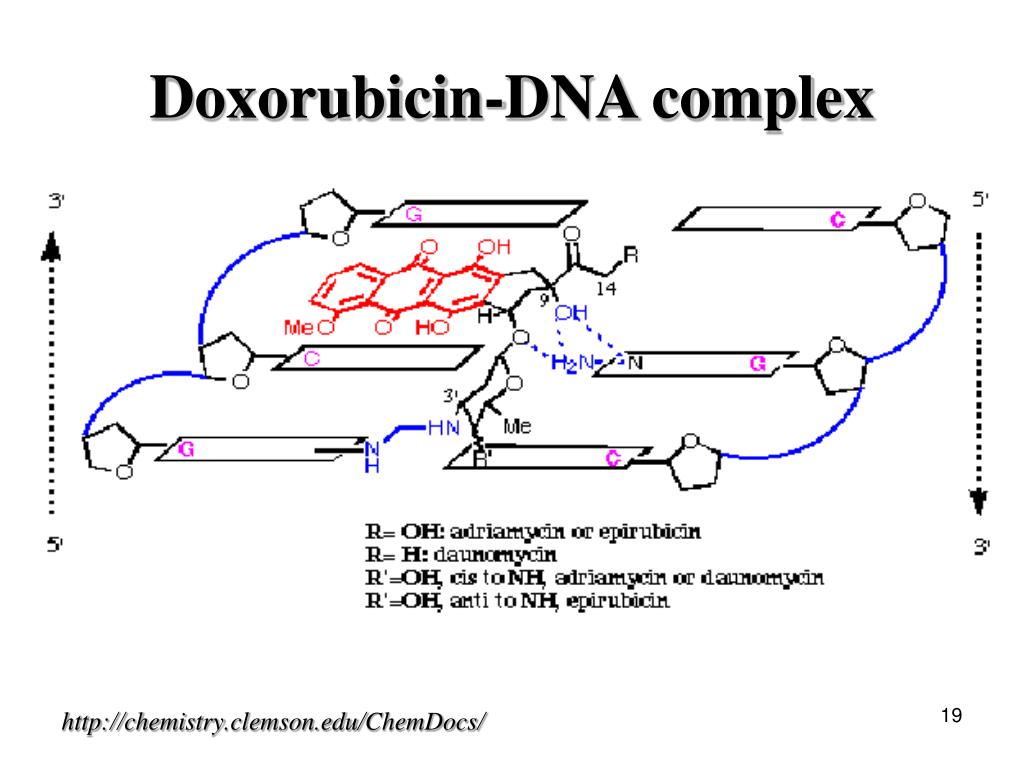
The data resulting from studies have shown that T-DM1 is a significant improvement in the treatment of advanced HER2-positive breast cancer. This can extend the life of patients previously treated with trastuzumab.ĭespite these advances, metastatic HER2-positive breast cancer remains incurable. With this in mind, the safety of T-DM1 was tested in a total of 1,871 patients with breast cancer in various clinical trials, with the following side effects being the most common: The most common reports of nausea, fatigue, and headache were reported by patients treated with this drug. This affected ≥25 percent. Side effects are all those effects of a drug that are not wanted or intended, but occur in the context of pharmacological treatment. Inhibiting tubulin prevents the cancer cell from dividing, which ultimately leads to its death through apoptosis. The results of the in vitro cytotoxicity tests showed that DM1 is between 20 and 200 times more potent than taxanes and vinca alkaloids. In addition, the mechanism of action of the cytostatic drug DM1 enables it to bind to tubulin.Like trastuzumab, T-DM1 is able to bind to HER2 / neu receptors and block the growth of tumor cells by inhibiting intrecellular signaling.So T-DM1 combines the mechanisms of action of these two drugs: Mechanism of action: What does T-DM1 do in the organism?Īs mentioned earlier, T-DM1 is a combination of two drugs: trastuzumab and DM1. In addition, the symptoms could be delayed significantly with treatment with T-DM1. The results of this study showed that affected patients lived longer, the progression of the disease could be delayed, and side effects could be better tolerated. Ī registry study called EMILIA compared treatment with T-DM1 with lapatinib and capecitabine in patients with this type of breast cancer who had previously been treated with a combination of trastuzumab and taxanes. To overcome this, trastuzumab-DM1 (T-DM1), a newer, more potent drug has been introduced. Despite encouraging clinical results, a significant fraction of patients are, or become, refractory to the drug. To date, only a combination of chemotherapy with capecitabine and lapatinib, a tyrosine kinase inhibitor of HER2 / ERGFR, has been recognized as a second-line treatment for advanced HER2-positive breast cancer. Introduction Trastuzumab is widely used for the treatment of HER2-positive breast cancer. First-line treatment of advanced HER-2 breast cancer with this medicine may improve the chances of survival.

In 2014, a second anti-HER2 drug came onto the market: pertuzumab. Before specific anti-HER2 therapies against this oncogene were developed, the prognosis for patients with HER2-positive tumors was worse than for other breast cancers.įortunately, however, the development of trastuzumab, a drug approved in 2000, has significantly improved the prognosis of HER2-positive metastatic breast cancer. Around 18 to 20 percent of women with breast cancer suffer from the HER2-positive metastatic type, which means that the HER2 receptor is produced in excess.


 0 kommentar(er)
0 kommentar(er)
